Canada
Alberta
University of Alberta
Edmonton, Alberta
View Details
Institution Name:
University of Alberta
Fellowship Program Name:
University of Alberta Reconstructive Urology Fellowship
Fellowship Program Location (City, State, Country):
Edmonton, Alberta, Canada
Fellowship Program Director Name:
Keith Rourke, MD, FRCSC Professor – Division of Urology University of Alberta Urology Site Chief – University of Alberta Hospital, Alberta Health Services
krourke@ualberta.ca
Fellowship Program Contact Person Name:
Tara Graham
urolpg@ualberta.ca
Fellowship Program Website Link:
https://www.ualberta.ca/surgery/divisions/urology/fellowship-programs/reconstructive.html
Length of Fellowship Program:
1 year
Fellowship Program Description:
The University of Alberta is one of Canada’s top teaching and research institutions and is located in the city of Edmonton, capital of the resource-rich province of Alberta. Our students, residents, and fellows have access to some of the most modern and well-equipped facilities in Canada.
This is a one-year clinical fellowship focusing on adult and pediatric urethral, bladder and genital urethral reconstructive surgery. The University of Alberta performs a high volume of reconstructive surgery and acts as the main reconstructive urology center for Western Canada. The fellowship program focuses on urethral reconstruction for stricture, hypospadias, fistula, and trauma as well as complex male genital reconstruction (trauma, Peyronie’s disease, lymphedema), surgery for sexual dysfunction (prostheses), complications of prostate cancer treatment and the adult neurogenic bladder. There is also a significant component of female pelvic floor reconstruction (stress incontinence, pelvic organ prolapse and voiding dysfunction). The fellow will participate in male and female reconstructive surgeries (>300 procedures/year) as well as perform pre-operative assessment, urodynamics and urethral imaging. This is a robust clinical fellowship with dedicated time and the expectation of clinical research with the opportunity for basic science research participation.
In a typical week, the fellow would attend 3 operative days per week with 1-2 days of ambulatory/office experience. The fellow will be actively scheduled with Dr. Keith Rourke (Male Reconstruction), Dr. Nathan Hoy (Male Reconstruction), Drs. Gary Gray, Joseph LaBossiere (Female Pelvic Medicine) and Derek Bochinski (Andrology). The fellow will regularly attend ambulatory clinics, cystoscopy urodynamics and operating rooms at the Kipnes Urology Centre, University of Alberta Hospital, Royal Alexandra Hospital and the Misericordia Hospital. The University of Alberta Hospital is also a Level 1 trauma centre and the fellow will be involved with select on-call cases.
It is expected that the fellow will actively pursue clinical research. Minimal expectations are submission of two abstracts to a major urology conference and prepare/submit at least one manuscript per year. The Fellow will also participate in weekly urology rounds, attend journal club and participate in other educational endeavors within the division. It is expected that the fellow will present at the Divisional of Urology Research Day.
Eligibility Requirements/Criteria (When Applicable):
The fellowship is open to those able to obtain post-graduate medical licensure in the province of Alberta or graduates outside of Canada who have external funding. Fellowship application is performed through the Society of Genitourinary Reconstructive Surgeons match (https://www.societygurs.org/gurs-fellowships-match/)
Requirements are:
1. Applicant should obtain post-graduate medical licensure and registration with the College of Physicians and Surgeons of Alberta (depending on funding source).
2. Registration with the Post-Graduate Medical Education (PGME) office at the University of Alberta ($945).
3. Applicant should have a valid work permit if not a Canadian citizen or permanent resident.
4. Membership with the Canadian Medical Protective Association (CMPA) as a clinical fellow.
5. Applicant must send a cover letter, current CV, and three reference letters supporting their application. One of these letters must be from the residency program director.
United States
California
Cedars Sinai Medical Center
Los Angeles, CA
View Details
Institution Name:
Cedars Sinai Medical Center
Fellowship Program Name:
The Gender Affirming Genital Reconstructive Surgery Clinical and Research Fellowship
Fellowship Program Location:
Los Angeles, CA USA
Fellowship Program Director Name:
Dr. Maurice Garcia
Fellowship Program Contact Person Name:
Soomie Chi
soomie.chi@cshs.org
Fellowship Program Website Link:
https://www.cedars-sinai.edu/education/graduate-medical/fellowship/female-pelvic-medicine-reconstructive-surgery.html
Fellowship Program Description / Overview:
The Gender Affirming Genital Reconstructive Surgery Clinical and Research Fellowship at Cedars-Sinai Medical Center offers a non-accredited: 1. One-year clinical and research program with a primary focus on a comprehensive list of all available feminizing or masculinizing genital surgeries (primary focus on one or the other, but with exposure to both); and 2. Two-year program to learn all surgical options for both feminizing and masculinizing surgeries.
Fellowships include a 12-month block of surgery and clinic activity within a high-volume tertiary care urology-led interdisciplinary transgender surgery and health program based within a leading academic medical center (hospital ranked # 2, and Urology program ranked #3 in nation, per U.S. News and World Report, 2022). Fellows have access to an NIH-funded research laboratory (R01CA201709-01; P.I. Garcia). Fellows participate in, and with time lead urology residents through all pre-operative, operative and post-op/long-term follow-up management of adult and adolescent patients. Specific surgeries fellows will learn to perform are shown below:
Adult and Pediatric clinical services:
- Longitudinal transgender genitourinary wellness care
- Transgender surgery care counselling for peds/adolescents and parents/guardians
- Peds/adolescent hormone-depot implant (in conjunction with the Program’s Peds endocrinologist)
- Pediatric and Adult Intersex GU wellness care
Genital surgeries offered at CSMC include:
Feminizing:
- Bilateral trans-scrotal orchiectomy (Urology)
- Vaginoplasty without and with creation of a vaginal canal by penile inversion technique, free scrotal skin grafts, or pedicle flaps (Urology)
- Revision surgeries of the vulva and/or urinary tract
- Primary Right-colon-vaginoplasty & salvage Right-colon vaginoplasty with neovaginectomy (*Urology and Colorectal surgery)
- Peritoneal vaginoplasty utilizing laparoscopic robot-assisted approach (*Urology)
Masculinizing:
- Metoidioplasty (Urology)
- Phalloplasty with and without urethral lengthening, using Radial Forearm Flap, Anterior
- Lateral Thigh Flap, Suprapubic and Groin flaps:
- First stage (Creation of phallus and urethra); (*Urology & Plastic Surgery)
Second stage: vaginectomy, urethral proximal urethroplasty, transposition of micro-penis into the phallus, scrotoplasty, and glansplasty (Urology)
- Implant of GU prosthetics (Urology)
- Salvage urethroplasty (Urology)
- Salvage phalloplasty, including Radial Artery Urethroplasty (Urology & Plastic Surgery)
Cedars Sinai Medical Center Cont.:
Gender non-conforming (non-binary) genital surgeries:
- Genital nullification surgeries
- Scrotectomy
- Vaginal-canal preserving phalloplasty and metoidioplasty
Adult Intersex / DSD (Disorders of Sexual Differentiation) surgeries:
- Primary and Revision pediatric and adult Intersex GU reconstructive surgeries
- Surgical collaboration with the CSMC Pediatric Surgery/Peds Urology teams for pediatric DSD surgeries
The fellowship program includes additional focus areas:
- Sexual medicine and neurourology
- Dedicated research time (clinical research with or without basic science research in our NIH-funded lab)
- A smaller but steady volume of cis-gender Men’s Health urologic surgeries (5-10% of practice; correction of penile curvature, GU prosthetics, GU reconstruction, male incontinence surgeries [AUS and slings], and Sexual Medicine)
- Program leadership training to prepare interested individuals to organize and lead a clinical transgender surgery program at another institution
- Clinic and operating room exposure to all core gender affirming surgery & medical specialty domains and faculty (e.g. Primary care clinic, Endocrinology/cross-sex hormone management clinic, Plastic surgery, Gynecologic surgery, ENT/Facial surgery, Dermatology, and Adolescent primary care and hormone management) [See: https://www.cedars-sinai.org/programs/transgender-surgery-and-health/services.html ]
- “Academic exchange” visits (in-person and virtual) with experts in the field in the USA and abroad
Academic urology support / environment:
- CSMC Urology residency program
- CSMC Urology fellowships, other: FPMRS
- Weekly Urology Grand Rounds and Morbidity and Mortality Conferences
- Biostatistician support
- Transgender Surgery and Health Program dedicated research assistant
- Membership support for AUA, Western Section AUA, USPATH, WPATH, and LACPATH
University of California at San Diego
San Diego, CA
View Details
Institution Name:
University of California, San Diego
Fellowship Program Name:
Genito-Urinary Reconstruction
Fellowship Program Location (City, State, Country):
San Diego, California, USA
Fellowship Program Director Name:
Jill C. Buckley, MD, FACS
Fellowship Program Contact Person Name:
Adela Lopez
alopez@health.ucsd.edu
Fellowship Program Website Link:
https://societygurs.org
Length of Fellowship Program:
1 year
Fellowship Program Description:
The fellowship is one clinical year focused on complex genito-urinary reconstruction including urethral reconstruction, ureteral reconstruction, urinary diversion, male incontinence surgery, fistula repair (rectourethral, vesicovaginal, vesical, and cutaneous fistula), hypospadias surgery, and complex genital reconstruction. There is a strong emphasis on robotic reconstructive techniques including the upper (ureteral reconstruction, nephrectomy) and lower urinary tract (bladder neck reconstruction, simple cystectomy, simple prostatectomy, ureteral reimplant). We use a wide range of techniques for both open and robotic surgery including anastomotic repairs, grafting, flaps, and combination techniques. We perform a high number of male incontinence surgeries, many of which are complex and redo cases. The program is based at the newly constructed UC San Diego Jacobs Medical Center in La Jolla with additional extensive exposure to our Level 5 Trauma center at UCSD Hillcrest.
The fellow will interact, teach and mentor the UCSD residents and medical students. They will have an independent clinic once a week caring for patients and scheduling operative cases independently. The remainder of the week will be in the operating room and clinic with the fellowship program director. Throughout the year, the fellow will participate in academic conferences and will have the opportunity to meet and interact with the other UC San Diego faculty. It is expected that the fellow will actively pursue clinical research with a half day per week of dedicated time.
Eligibility Requirements/Criteria (When Applicable):
1. Applicant must send a cover letter, current CV, and three reference letters supporting their application. One of these letters must be from the residency program director to establish good standing.
2. Admission is contingent upon completion of an ACGME accredited urologic training program.
3. Applicant should have successfully completed all 3 steps of USMLE and be eligible for California state medical licensure.
University of California at Irvine
Orange, CA
View Details
Institution Name:
University of California, Irvine
Length of Fellowship Program: 1 year (optional 2 years with an enhanced and expanded research and clinical experience)
Fellowship Overview: The Endowed Eric S. Wisenbaugh GURS Fellowship in Reconstructive and Prosthetic Urology at UC Irvine is a one-year clinical Fellowship located in idyllic Orange County California emphasizing urethral and genital reconstructive surgery including penile curvature correction surgery and hypospadias repair, penile prosthesis surgery, Men’s health, bladder and upper tract reconstruction, male incontinence treatment, and cancer survivorship. NIH-funded tissue engineering research is also provided for those pursuing a two-year program.
Program Highlights:
- Training in urethroplasty, penile-genital reconstruction, genitourinary prosthetics and complex abdominal and upper tract surgeries.
- Affiliated hospitals: UC Irvine Medical Center, Long Beach VA Medical Center, Children’s Hospital of Orange County (CHOC).
- Full-time Research coordinator managing a prospectively-maintained Reconstructive Urology Database to support clinical research productivity. This database contains over 3,400 cases of reconstructive surgery performed over a 26-year period of patients who travelled to our Center from 46 states and 34 countries.
Clinical Training:
- Urethroplasty: Posterior urethroplasty for PFUI and radiation strictures, bulbar anastomotic urethroplasty, substitution urethroplasty for bulbar, penile, and/or fossa navicularis strictures, pan-urethral repairs, revision urethroplasty, lichen sclerosus treatment, and hypospadias repairs. Over 200 imaging procedures are performed annually (retrograde urethrograms and cystourethrograms).
- Penile Reconstruction: Peyronie’s disease repair, congenital curvature correction, penile implants (including complex revisions), and scrotal reconstruction.
- Ureteral Reconstruction: Pyeloplasty, Complex ureteral reconstruction using flaps and grafts, Ureteral reimplantation.
- Bladder and Bladder Neck Reconstruction: Bladder neck reconstruction, non-cancer cystectomies, continent and incontinent urinary diversion and augmentation. Patient population: Male and Female neurogenic, cancer survivorship, trauma and infection related patients.
- Men’s Health: Office procedures (e.g., penile duplex doppler, collagenase administration).
- Robotic and Open Surgery opportunities: Our surgical approaches include open, robotic single port and multi-port options including ureteral stricture repair.
Unique Opportunities:
- Funded 2-week trip to HCMC, Vietnam and potential additional travel toBangkok, Thailand for reconstructive workshops with a focus on anastomotic bulbar and posterior urethroplasty.
- Optional one-week proctorship at an international center of excellence focused on prosthetic urology.
- Attendance at major urological conferences (AUA, SMSNA, Western-Section AUA, GURS) without limitation when the Fellow is presenting accepted abstracts.
Eligibility:
- U.S. Citizenship highly desirable (due to VA Hospital affiliation).
- California Medical License needed before July 1, 2026.
Program Leadership:
- Fellowship Directors: Dr. Joel Gelman, Professor of Urology and Chief of the Division of Reconstructive Urology and Dr. Keith Rourke, Professor of Urology
- Additional Faculty: Dr. Zhina Sadeghi (Bladder-Abdominal and Upper Urinary tract Reconstruction), Dr. Faysal Yafi (Men’s Health), Dr. Antoine Khoury (Pediatric Urology), and other Faculty.
- Research Laboratory: Directed by Dr. Joshua Mauney, Endowed Presidential Chair in urethral-genital tissue bioengineering.
Funding & Resources:
- Supported by a $1,000,000 Endowment and additional funds.
- No General Urology clinic duties or call coverage required.
- Dedicated time for academic pursuits and international outreach.
Past Fellow Achievements:
2014-2015 Dr. Justin Degrado, Captain US Navy, Fellowship sponsored by the Navy to prepare Dr. Degrado to serve in a Reconstructive Urology leadership role, including the Navy Urology Residency Program
2015-2016 Dr. Eric S. Wisenbaugh, Assistant Professor, University of Oklahoma (deceased)
2016-2017 Dr Kristi Hebert, Private Practice Atlanta, Georgia 2016-7
2018-2019 Dr. James Furr, Assistant Professor, University of Oklahoma
2019-2020 Dr. Aron Liaw, Assistant Professor, Wayne State Univeristy
2020-2021 Dr. John Barnard, Assistant Professor, University of West Virginia
2021-2023 Dr. David Barham, Major US Army. Dr. Barman was sponsored for a 2-year Fellowship in preparation for a leadership position in the US Army. He is now Faculty at Brooke Army Medical Center. His 2-year experience included 109 urethroplasty cases, 111 penile implant cases, 34 genital reconstructive surgeries, 26 publications, and 8 AUA presentations
2023-2024 Dr. Babak Azad, Assistant Professor, Tulane University
2024-2025 Dr. Jeffrey Lee, Current Fellow, anticipated post-Fellowship position, Assistant Professor, Stony Brook, New York
2025-2026 Dr. Seth Thomas, anticipated post-Fellowship position, Assistant Professor, University of Michigan Sparrow Hospital
- Training Volume & Scope
|
Procedure Type |
Annual Volume |
Key Techniques |
|
Urethral Imaging |
200+ * |
Retrograde urethrograms, cystourethrograms. |
|
Urethral Reconstruction |
80+ * |
Includes complex cases |
|
Graft Harvesting |
50+ * |
Buccal, lingual mucosa, split-thickness skin. |
|
Penile Implant Surgery |
80+ |
Includes complex revision cases. |
|
Ureteral & Bladder Reconstruction |
30+ * |
Includes complex cases, cancer survivorship, revision cases |
* Current and past-case logs represent an underestimation of the urethral-genital and upper tract reconstructive surgery ocase volume that is anticipated starting in July, 2025. Our Faculty expanded 2-years ago with the addition of Dr. Zhina Sadeghi, who is Fellowship Trained and experienced a rapid growth in abdominal and upper tract reconstructive surgery volume. Dr. Sadeghi’s case volume does not include penile or urethral reconstructive surgery and therefore, her clinical focus is predominantly abdominal and upper tract cases, which will be supported by a Presidential Endowed Chair.
In addition, Dr. Keith Rourke will join our Fellowship Program in July, 2025 as a Program Co-director, and it is anticipated that our urethroplasty and genital surgery case volume will double.
University of California at San Francisco
San Francisco, CA
View Details
Institution Name:
University of California at San Francisco (UCSF)
Fellowship Program Name:
Male Genitourinary Reconstruction and Trauma Fellowship
Fellowship Program Location (City, State, Country):
San Francisco, California, USA
Fellowship Program Director Name:
Benjamin N. Breyer, MD, MAS, FACS
bbreyer@urology.ucsf.edu
Fellowship Program Contact Person Name:
Karen Tabayoyong
Karen.Tabayoyong@ucsf.edu
Fellowship Program Website Link:
https://urology.ucsf.edu/education/fellowships/male-genitourinary-reconstruction-trauma
Length of Fellowship Program:
1 year
Fellowship Program Description:
The UCSF Male Genitourinary Reconstruction and Trauma Fellowship program is a mentored, graduated experience in trauma diagnosis and management primarily based on Zuckerberg San Francisco General Hospital and Trauma Center (ZSFG). This provides the fellow an opportunity to work as a member of a Trauma Team providing care for acute trauma to the urinary and genital system. Fellows are supervised and guided through the development of research projects, which include protocol preparation and development, statistical analysis, data collection techniques, data interpretation, manuscript preparation, etc. It is expected that each trainee will complete and publish numerous manuscripts during fellowship.
Aside from the clinical and academic research experience, the program seeks to attract bright, committed, and compassionate applicants from diverse backgrounds, who aspire to become future leaders in this specialty. They should possess a desire to serve culturally diverse and medically underserved populations while being dedicated to addressing issues related to diversity, equity, and inclusion. The program also focuses in honing leadership qualities to prepare the fellow for future leadership roles in academic medicine.
Eligibility Requirements/Criteria (When Applicable):
• Candidate must have completed an ACGME Urology Residency Training Program
• Candidate must be a US citizen due to the funding of the position
• Special interest in future academic and scholarly activities is considered highly favorable
• Preferably be a candidate for the American Board of Urology
• Candidate must be eligible to obtain a California medical license (please refer to the CA Medical Board for eligibility requirements)
Application Packets should include:
• Cover Letter
• GURS AUA application
• Curriculum Vitae
• A headshot photo (jpeg)
• (3) three letters of reference
Colorado
University of Colorado School of Medicine
Aurora, CO
View Details
Institution Name:
University of Colorado School of Medicine, Anschutz Medical Campus
Fellowship Program Name:
Functional & Reconstructive Urology Fellowship
Fellowship Program Location (City, State, Country):
Aurora, Colorado, USA
Fellowship Program Director Name:
Brian Flynn, MD
brian.flynn@ucdenver.edu
Fellowship Program Contact Person Name:
Shannon Lamoree
shannon.lamoree@cuanschutz.edu
Fellowship Program Website Link:
https://medschool.cuanschutz.edu/surgery/divisions-centers-affiliates/urology/education/genitourinary-reconstructive-fellowship/overviewhttps://medschool.cuanschutz.edu/surgery/specialties/urology/education/genitourinary-reconstructive-fellowship
Length of Fellowship Program:
2 years (first year research, second year clinical)
Fellowship Program Description:
Fellowship will focus on reconstructive urologic surgery including pre-operative evaluation, intraoperative management with familiarity in reconstructive techniques, instrumentation, and post-operative management and care.
Areas of emphasis are: The management of Male Stress Urinary Incontinence and proficiency in artificial urinary sphincter, sling, proACT. Penile Reconstruction for Peyronie’s Disease and erectile dysfunction. Management of urethral stricture disease including urethroplasty using grafts and flaps. Fellow will be proficient in management of GU fistulas.
Fellow will demonstrate knowledge in ureteral reconstruction and be adept in the full array of reconstructive procedures including ureteral re-implantation, uretero-ureterostomy, transuretero-ureterostomy, ileal uretero substitution, boari flap, and pyeloplasty and diversion (both open and robotic). Bladder reconstruction including bladder augmentation, creation of catheterizable urinary stomas, urinary diversion.
Eligibility Requirements/Criteria (When Applicable):
Applicant must be eligible for a Colorado State medical license prior to start of the fellowship. This fellowship is open to both “U.S. citizens” and “non-U.S. citizens”.
Applicant should have completed all 3 steps of USMLE.
Applicant must have three letters supporting his application for fellowship. One of these letters must be from his current program director.
Illinois
Loyola University Medical Center
Maywood, IL
View Details
Institution Name:
Loyola University Medical Center
Fellowship Program Name:
Genitourinary Reconstruction and Male Pelvic Health Fellowship
Fellowship Program Location:
Maywood, IL USA
Fellowship Program Director Name:
Chris Gonzalez, MD, MBA, FACS
Fellowship Program Contact Person Name:
Susan Di Salvo
sdisalvo@lumc.edu
Length of Fellowship Program:
1 year
Fellowship Program Website Link:
https://www.loyolamedicine.org/gme/fellowships/urology/male-pelvic-health-genitourinary-reconstruction
Fellowship Program Description:
Loyola University Medical Center (LUMC) and affiliate hospitals, Gottlieb Memorial Hospital (GMH) and MacNeal Hospital (MNH) are a regional referral centers of reconstructive urology for the Chicago metro. The fellowship is a one-year clinical fellowship designed to provide expertise in adult reconstructive urology with special focus on: urethral stricture disease, hypospadias failure, buried penis repair, male urinary incontinence, erectile dysfunction and Peyronie’s disease. This includes a broad range of surgical procedures including urethroplasty, artificial urinary sphincter placement, male urethral slings, penile prosthesis insertion, buried penis repair with skin grafting, penile plication, penile incision and grafting, modern procedural management of BPH, varicocelectomy and vasovasostomy with an expanding case load of infertility management. There is also large volume of abdominal and robotic reconstructive cases performed which include urinary diversion for devastated lower urinary tract, ureteral reconstruction and bladder neck reconstruction for refractory stenosis. There is also a good exposure to trauma as LUMC is a Level 1 Trauma center and GMH and MNH are both Level 2 Trauma centers.
Faculty:
Christopher Gonzalez, MD, MBA, FACS
Program Director
Ahmer Farooq, DO, FACS
Men’s Health and Sexual Medicine
Ahmad El-Arabi, MD
Genitourinary Reconstruction
Kevin McVary, MD, FACS
Men’s Health and Sexual Medicine
Denise Asafu-Adjei, MD, MPH
Andrology and Infertility
Clinical Responsibilities:
The fellow will function as a clinical instructor with hospital staff privileges and take call once every 2-3 months. The fellow will run an independent clinic approximately one half-day per week. The fellow operates 3 days per week and spend 1.5 days per week in our reconstruction clinic.
Academic Opportunities:
The fellow will have the opportunity to interact routinely with residents and medical students in both an operative and didactic capacity. This includes research mentorship and involvement in ongoing research endeavors with program faculty.
Eligibility Requirements/Criteria:
- Applicants must send a CV, letter of interest, and 3 letters of recommendation supporting their application. One letter must be from the program director establishing good standing within their residency program.
- Completion of ACGME accredited urologic training program.
- Successful application for medical licensure in the State of Illinois.
Iowa
University of Iowa
Iowa City, IA
View Details
Program: Genitourinary Reconstruction
Contact Person: Bradley A Erickson, MD
Email: brad-erickson@uiowa.edu
Phone: 319-356-7221
Fax: 319-356-3900
OR
Theresa Lent
Fellowship Coordinator
Email: theresa-lent@uiowa.edu
Phone: 319-353-8939
Fax: 319-356-3900
MAILING ADDRESS:
University of Iowa Hospitals & Clinics
Department of Urology
200 Hawkins Drive
Iowa City, IA 52242-1089
Website: https://uihc.org/urology-clinic
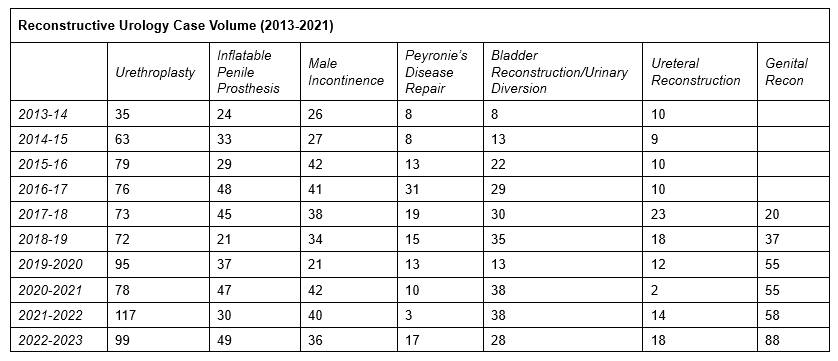
History:Dr. Karl J. Kreder started the reconstructive urology fellowship at the University of Iowa in 1997. Since its inception, a total of 20 fellows have been trained at Iowa. In 2014, Dr. Bradley A. Erickson was named the fellowship director, and the emphasis of the fellowship program has shifted from female/male pelvic reconstruction, to male pelvic reconstruction, prosthetics, and transgender surgery. In 2019, the University of Iowa began to offer transgender surgical care including gender affirming bottom surgery. In 2023, Dr Amanda Swanton joined the faculty, providing the fellowship with added emphasis on Men’s Health and transgender care.
Recent Genitourinary Reconstruction Fellows
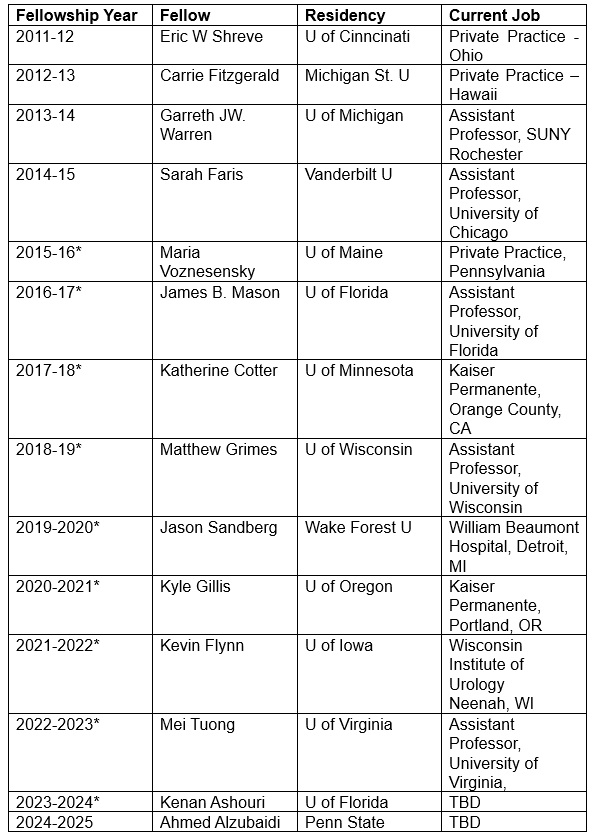
*Boston Scientific Fellowship Grant Recipient
Duration: 12 months. Applicants interested in a 24-month fellowship that would include 12 months of clinical and/or basic science research should alert Theresa Lent at the time of application submission. The research year would commence in the second year of the fellowship.
Goals and Objectives for Training:
The overall mission of the fellowship program is to provide 12 months of intense, comprehensive clinical and surgical training in urologic reconstruction and urologic prosthetics that prepares the fellow for a practice that focuses on meeting the unique reconstructive needs of patients. The fellowship provides extensive hands-on training in the operating room, where it is expected that fellows will be able to independently perform both routine cases and cases of moderate complexity that deal with aspects of male reconstruction (e.g. urethral stricture, erectile dysfunction, stress incontinence) and general reconstruction (urinary diversion, ureteral reconstruction, surgery in previously operated/radiated fields) at the completion of the year. The fellowship also involves training in counseling patients regarding and performing transfeminine gender-affirming genital surgery. The fellow will also become proficient in the clinical work-up and management of men’s health issues by working directly with Dr. Erickson and Dr Swanton, also by conducting their own, independently run clinic that focuses on reconstructive cases. Finally, the fellow will become proficient in designing and conducting clinical research projects that deal with reconstructive urology and men’s health. Importantly, the fellow will have access to the Trauma and Urologic Reconstruction Network of Surgeons (TURNS) database, a database which has to date led to over 70 manuscripts published in peer-reviewed journals. TURNS is made up of 14 fellowship trained surgeons. A research website (www.turnsresearch.org) is maintained by the TURNS group.
Program Certifications: None
Teaching Staff
Key Program Faculty:
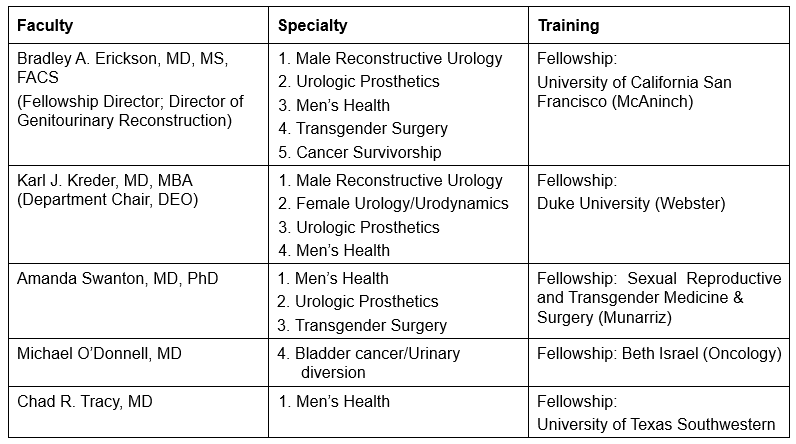
Facilities: The fellow will work at the University of Iowa Hospitals & Clinics, the Iowa City Veteran’s Hospital and the Iowa River Landing outpatient facility.
Educational Program, Basic Curriculum:
Historical Case Volume – University of Iowa
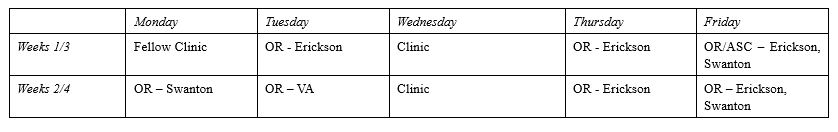
Learning Activities/Didactic Teach Sessions – University of Iowa
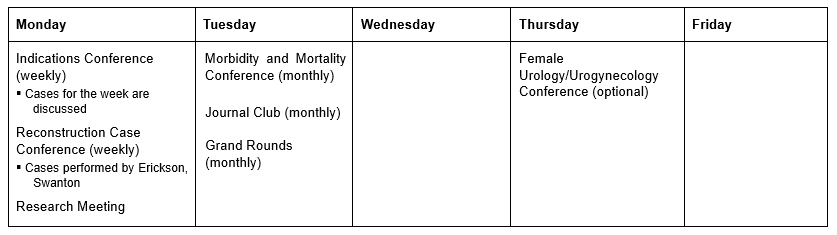
Monthly Schedule
Prerequisite/Eligibility Criteria:
- Admission is contingent upon completion of an ACGME accredited residency training program in urology. In special circumstances, qualified candidates who have completed their formal training in foreign countries and who have completed the requirements for foreign graduates may also apply.
- Applicant must have completed all three steps of USMLE.
- Applicants must have three letters supporting his/her application for fellowship. One of these letters must be from his/her current program director.
- Applicant must be eligible for a permanent Iowa medical license prior to the start of their fellowship. Learn more about eligibility requirements on the Iowa Board of Medicine website.
- Foreign applicants are responsible for obtaining appropriate visas prior to the scheduled start of the fellowship. The fellowship is preferentially offered to those who are considered for a staff position at an academic program nationally or internationally or who intend to pursue an academic career in urology.
Submission Materials:
- Qualified applicants please submit application, CV, personal statement & photo to Dr Brad Erickson & Theresa Lent.
Massachusetts
Lahey Hospital and Medical Center
Burlington, MA
View Details
Institution Name:
Lahey Hospital and Medical Center
Fellowship Program Name:
Genitourinary Reconstructive Surgery
Fellowship Program Location (City, State, Country):
Burlington, Massachusetts, USA
Fellowship Program Director Name:
Alex J. Vanni, MD, FACS
Fellowship Program Contact Person Name:
Alex J. Vanni
alex.j.vanni@lahey.org
Fellowship Program Website Link:
https://www.lahey.org/lhmc/department/urology/reconstructive-urologic-surgery/
Length of Fellowship Program:
1 year
Fellowship Program Description:
The Center for Reconstructive Urologic Surgery is a regional, national, and international referral center founded by Dr. Leonard Zinman in 1973. The fellowship is a one-year clinical position, designed to provide expertise in adult reconstructive urology including: urethral reconstruction, hypospadias, rectourethral fistula repair, robotic and open ureteral reconstruction, buried penis repair, genital skin grafting, primary and revision gender affirming surgery, Peyronie’s disease, genital lymphedema, surgery for penile and urethral cancer, as well as GU prosthetic cases (AUS, male sling, IPP).
Fellows will participate in a high-volume reconstructive practice with over 500 cases a year to choose from and GURS case logs consisting of ~300 procedures per year (> 125 urethral reconstructions per year). In addition to a large surgical volume, fellows will participate in a weekly reconstruction clinic gaining experience in preoperative decision making and urethral imaging.
Goals and Objectives for Training:
This fellowship provides robust exposure to complex reconstructive urologic and prosthetic surgery. The fellow will attain graduated responsibility in the operating room throughout the year. The goal of training is to obtain expertise in the pre-operative, operative, and post-operative management of adult reconstructive urology. Additionally, clinical research, surgical education and mentoring are emphasized with the goal of training individuals for a future academic career in reconstructive urology.
Faculty:
Alex J. Vanni, MD, FACS
Program Director
Khushabu Kasabwala, MD
Reconstruction and Gender-Affirming Surgery
Andrew McCullough, MD
Men’s Health and Sexual Medicine
Alireza Moinzadeh, MD
Division Chair and Chief of Robotic Urologic Surgery
Clinical Responsibilities:
The fellow needs to obtain a Massachusetts medical license and will function as a clinical instructor with hospital staff privileges. The fellow will run an independent clinic approximately 3 days per month. The fellow operates 3-4 days per week and spend 1 day per week in our reconstruction clinic.
Research:
Fellows will have the opportunity to participate in clinical research through Lahey Hospital and Medical Center, as well as participate in outcomes studies with the Trauma and Urologic Reconstruction Network of Surgeons (TURNS) database.
Fellows will be expected to submit at least 2 abstracts to a regional or national meeting, and to submit at least one manuscript for peer-reviewed publication. Support is provided for travel to the annual meeting of the American Urological Association.
Teaching:
Fellows will supervise residents in the operating room and are expected to participate in weekly departmental conferences including morbidity and mortality, GU radiology, indications, journal club and Grand Rounds.
Eligibility Requirements/Criteria (When Applicable):
1. Must be eligible for medical licensure in the state of Massachusetts prior to starting fellowship and be a United States citizen.
2. Admission is contingent upon completion of an ACGME accredited urologic training program.
3. Applicant should have completed all 3 steps of USMLE.
4. Applicant must have 3 letters of support for fellowship. One of these letters must be from his/her current program director.
5. Applicant must be a US citizen
Minnesota
Mayo Clinic School of Graduate Medical Education
Rochester, MN
View Details
Institution Name:
Mayo Clinic School of Graduate Medical Education
Fellowship Program Name:
Trauma and Genitourinary Reconstruction Fellowship
Fellowship Program Location:
Rochester, MN USA
Fellowship Program Director Name:
Dr. Boyd Viers
Viers.Boyd@mayo.edu
Fellowship Program Contact Person Name:
Megan Braski
Braski.Megan@mayo.edu
Fellowship Program Website Link:
https://college.mayo.edu/academics/residencies-and-fellowships/trauma-and-genitourinary-reconstruction-fellowship-minnesota/
Length of Fellowship Program:
1 year
Fellowship Program Description:
The one-year Trauma & Genitourinary Reconstruction Fellowship program at Mayo Clinic in Rochester, Minnesota, provides advanced clinical and surgical training to develop a thorough understanding of the evaluation and management of a broad spectrum of disorders, preparing graduates to provide comprehensive, individualized diagnosis and treatment for a variety of reconstructive urologic conditions.
Utilizing a 1:1 mentorship model, the clinical year consists of six sequential 8–9-week rotations with 3 GURS trained faculty members. Rotations provide a comprehensive experience, and advanced training, in complex facets of procedures, pathologies, and case management. Experience includes both complex open surgery and advanced robotic reconstruction. Fellows will treat a high volume of male urethral stricture disease (using open, robotic, and endoscopic approaches), genitourinary fistula, ureteral stricture disease, and male stress urinary incontinence. The program provides in-depth exposure and training involving the complexities of multi-disciplinary genitourinary reconstruction and cancer survivorship. The fellow gains experience and competency in the surgical management of patients with neurogenic bladder, acquired buried penis, and gender affirming surgery.
The fellow participates in weekly imaging and pathology case conferences, dedicated biweekly reconstructive urology indications conference, as well as a monthly reconstructive urology Journal Club. Mayo Clinic’s Trauma & Genitourinary Reconstruction Fellowship program actively supports research through faculty mentorship, robust statistical support, database management, and travel to regional and national meetings to present research. International outreach opportunities are also available.
Eligibility Requirements/Criteria:
To be eligible for the Trauma & Genitourinary Reconstruction Fellowship program, candidates must have completed a residency program in urology in the United States or Canada that is accredited by the Accreditation Council for Graduate Medical Education (ACGME) or the Royal College of Physicians & Surgeons of Canada (RCPSC) and be eligible for a Minnesota medical license.
Qualified candidates from outside the United States and Canada must meet the following criteria:
Meet all visa sponsorship requirements
Be certified by the Educational Commission for Foreign Medical Graduates (ECFMG)
Be eligible for a Minnesota medical license, which requires a minimum of one year of accredited residency or fellowship training in the United States or Canada
Qualified candidates must also meet all general admissions requirements for the Mayo Clinic School of Graduate Medical Education.
University of Minnesota
Minneapolis, MN
View Details
Institution Name:
University of Minnesota
Fellowship Program Name:
Urology Reconstructive Fellowship Program
Fellowship Program Location (City, State, Country):
Minneapolis, Minnesota USA
Fellowship Program Director Name:
Sean Elliott, MD, MS
selliott@umn.edu
Fellowship Program Contact Person Name:
Liz Mayock
eamayock@umn.edu
Fellowship Program Website Link:
https://med.umn.edu/urology/education-training/fellowships/reconstructive-fellowship
Length of Fellowship Program:
1 year
Fellowship Program Description:
The University of Minnesota, Department of Urology offers a 1-year GURS clinical fellowship in genitourinary reconstructive surgery. The Urology Reconstructive Fellowship program is led by Drs. Sean Elliott and Joseph Pariser and has been in operation since 2013.
Our fellowship program emphasizes male urethral reconstruction, male urinary incontinence surgery, ureteral stricture repair, genital reconstruction including skin grafting, gender affirmation surgery and has a major emphasis in complex neurogenic bladder management. Robotic and laparoscopic techniques are used often.
The fellow has hospital staff privileges and takes call on the same schedule as the faculty (approximately 1 week in 8). They have a clinic of their own at the University for 0.5 to 1 days a week. They also come with us to our affiliated Gillette Lifetime Clinic where we care for adults with congenital urologic issues, such as spina bifida and cerebral palsy. The fellow participates in the operating room with Dr. Elliott or Dr. Pariser at least 3 days per week. The fellow gains graduated responsibility throughout the year in both the clinic and the operating room.
We provide excellent resources and mentoring for success in research. Fellows typically complete about 3 projects during their year here. Recent fellows have launched careers at Cleveland Clinic (2022), Lahey Clinic (2021), Mayo Clinic (2020) and Indiana University (2019).
Eligibility Requirements/Criteria (When Applicable):
Admission is contingent upon completion of an ACGME-accredited urology training program.
The applicant must be a US citizen.
The applicant must have three letters of support, including one from their chairperson.
The applicant must have passed all 3 steps of USMLE before the match date and be eligible for a Minnesota State medical license prior to starting fellowship.
Missouri
Washington University School of Medicine in St. Louis
St. Louis, MO
View Details
Institution Name:
Washington University School of Medicine in St. Louis
Fellowship Program Name:
Trauma and Reconstruction Fellowship
Fellowship Program Location:
Fellowship Program Director Name: Dr. Gregory Murphy
Meetings and Education:
Fellowship Program Location: St. Louis, MO, USA
Fellowship Program Director:
Gregory Murphy, MD
murphyg@wustl.edu
Fellowship Program Coordinator:
Gina Yu
urologyeducation@wustl.edu
314-362-8028
Fellowship Program Website Link:
https://urology.wustl.edu/education/fellowships/urologic-trauma-and-reconstruction-fellowship/
Fellowship Program Description / Overview:
The fellowship is a one-year clinical position, beginning August 1st, designed to provide expertise in reconstructive urology at Washington University. Common conditions include: urethral stricture disease, male incontinence, erectile dysfunction, Peyronie’s disease, ureteral strictures, hypospadias, rectourethral fistula, buried penis, GU trauma, transitional urology, transgender surgery, neurogenic bladder, infertility and female urology.
Faculty:
Dr. Gregory Murphy completed a fellowship in trauma and male reconstruction at University of California, San Francisco and specializes adult male reconstructive surgery.
Other faculty include:
Dr. Charlie Jones who specializes in male reconstruction and transitional surgery.
Dr. Dane Johnson who specializes in ED, Peyronie’s, infertility and mircrosurgery.
Dr. Henry Lai who specializes in female urology and voiding dysfunction.
In addition to a large surgical volume, fellows will participate in reconstruction clinic, gaining experience in preoperative decision making.
Goals and Objectives for Training:
This fellowship provides robust exposure to complex male reconstructive urologic surgery with flexibility for training in infertility, congenitalism, and female urology depending on interest. The fellow will attain graduated responsibility in the operating room throughout the year. Additionally, clinical research, surgical education and mentoring are emphasized.
Clinical Responsibilities:
The fellow will function as a clinical instructor with hospital staff privileges and be part of the attending call pool.
Research:
The fellow will have the opportunity to participate in clinical research. Washington University Urology has significant staff support for research and multiple reconstruction databases.
Eligibility Requirements/Criteria
1. Must be eligible for medical licensure in the state of Missouri prior to starting fellowship.
2. Admission is contingent upon completion of an ACGME accredited urologic residency or appropriate foreign program.
3. Applicant should have completed all 3 steps of USMLE.
4. Applicant must have 3 letters of support for fellowship. One of these letters must be from his/her current program director.
5. Current CV
New York
Mount Sinai Hospital
New York, NY
View Details
Institution Name:
Mount Sinai Hospital
Fellowship Program Name:
Fellowship in Reconstructive Urology and Gender Affirmation Surgery
Fellowship Program Location (City, State, Country):
New York, New York, USA
Fellowship Program Director Name:
Rajveer Purohit, MD, MPH & Miroslav Djordjevic,MD, PhD
Fellowship Program Contact Person Name:
Rajveer Purohit
rajveer.purohit@mountsinai.org
Fellowship Program Website Link:
https://icahn.mssm.edu/education/residencies-fellowships/list/reconstructive-urology-fellowship
Length of Fellowship Program:
1 year
Brief Description of Fellowship Program:
Mount Sinai offers a large volume reconstructive urology training program for the fellow centered on gender affirmation surgery but with a robust complement of most other types of reconstructive and robotic urological surgeries. The program provides training at a regional referral center with a very large volume in complex reconstructive urology.
A fellowship is directed by Dr. Rajveer Purohit and the fellow will spend her/his time primarily with him, Dr. Miroslav Djordjevic, Dr. Gregory Amend and Dr. Robert Valenzuela. The fellow will be in the operating room 4 days a week with 2-3 days spent assisting in the OR with gender affirmation surgery and 1-2 days will be focused on other reconstructive surgeries. 1 day a week will be spent in a clinic focused on pre-operative and post-operative management of reconstructive cases. Fellows will learn to teach residents and gain increasing surgical autonomy as they progress through the year.
The heart of our program is focused on gender affirming surgery but our program offers a tremendous variety of procedures in all other aspects of reconstructive urology including a high volume of urethral and genital reconstruction, prosthetics, buried penis and robotic bladder neck and upper tract surgery. The large number of open and robotic cases and their high degree of complexity will be a significant driver of acquiring new skills and experience for the fellow.
The curriculum of gender affirmation surgery includes primary vaginoplasty, phalloplasty (utilizing both free flap and local flaps), metoidioplasty, and revision surgeries. Almost all gender affirmation surgeries are done without the assistance of the plastic surgery team. In addition, a busy practice is maintained in urethral reconstruction, prosthetics, Peyronie’s disease, treatment of male stress urinary incontinence, urinary fistulas, buried penis and robotic reconstruction of the bladder neck and ureter. Fellows will learn diagnosis and evaluation of these conditions, along with management strategies including behavioral and pharmacological treatment, sophisticated surgical solutions, and minimally invasive options.
More information can be found on our website:
https://icahn.mssm.edu/education/residencies-fellowships/list/reconstructive-urology-fellowship
Eligibility Requirements/Criteria (When Applicable):
Fellows must be eligible to practice medicine in the United States
NYU Grossman School of Medicine
New York, NY
View Details
Institution Name:
NYU Grossman School of Medicine
Fellowship Program Name:
Gender-Affirming & Reconstructive Surgery Fellowship
Fellowship Program Location (City, State, Country):
New York, New York, USA
Fellowship Program Director Name:
Lee Zhao, MD
Fellowship Program Contact Person Name:
Lee Zhao, MD
Lee.Zhao@nyulangone.org
Fellowship Program Website Link:
https://med.nyu.edu/departments-institutes/urology/education/gender-affirming-reconstructive-surgery-fellowship
Length of Fellowship Program:
1 year
Suny Upstate Medical University
Syracuse, NY
View Details
Institution Name:
SUNY Upstate Medical University
Fellowship Program Name:
SUNY Upstate Reconstructive Urology Fellowship
Fellowship Program Location (City, State, Country):
Syracuse, New York, USA
Fellowship Program Director Name:
Dmitriy Nikolavsky, MD
nikolavd@upstate.edu
Fellowship Program Contact Person Name:
Susan Schulze
schulzes@upstate.edu
Fellowship Program Website Link:
https://www.upstate.edu/urology/education/gurs-fellowship/index.php
Length of Fellowship Program:
1 year
Fellowship Program Description:
This is a 1-year Reconstructive Urology Fellowship through the Department of Urology at SUNY Upstate Medical University. The fellows will have the opportunity to operate at two sites: SUNY Upstate University Hospital Main Campus (primary site) and SUNY Upstate Community Hospital.
The program offers a combined clinical, operative and research training experience. Upon completion, fellows will be proficient in pre-operative evaluation, surgical intervention and post-operative care of genitourinary reconstructive patients.
Eligibility Requirements/Criteria (When Applicable):
1. Applicant must be eligible for a New York State medical license prior to start of the fellowship.
2. This fellowship is open to both “U.S. citizens” and “non-U.S. citizens”.
3. Applicant should have completed all 3 steps of USMLE and be Board Eligible
4. Applicant must have three letters supporting his application for fellowship. One of these letters must be from their current program director.
North Carolina
Duke University Medical Center
Durham, NC
View Details
Institution Name:
Duke University
Fellowship Program Name:
Reconstructive Urology and Genitourinary Cancer Survivorship
Fellowship Program Location (City, State, Country):
Durham, North Carolina, USA
Fellowship Program Director Name:
Andrew C. Peterson, MD, MPH, FACS
Fellowship Program Contact Person Name:
Apryle M. Graham
apryle.graham@duke.edu
Fellowship Program Website Link:
https://surgery.duke.edu/education-and-training/fellowship-programs/reconstructive-urology-and-genitourinary-cancer-survivorship
Length of Fellowship Program:
1 year
Fellowship Program Description:
This fellowship provides a heavy emphasis on clinical experience exposing the fellow to routine and complex cancer survivorship reconstructive urologic conditions. This exposure includes education in the multidisciplinary approach to cancer survivorship reconstructive urologic care. This includes exposure to radiation oncology, colorectal surgery, surgical oncology, medical oncology, andrology, male reconstructive urology, urodynamics and some pediatric urologic care. Fellows will participate in the multidisciplinary clinics with exposure to the disciplines of both male and female reconstruction to include fistula working group, osteomyelitis working group and genitourinary cancer survivorship clinic. Surgical training will include both advanced exposure to both minimally invasive and open surgical procedures as well as prosthetics and incontinence procedures. The end goal is production of a clinical specialist with emphasis on genitourinary cancer survivorship for placement in academic training facilities with association with a cancer center. The graduate will have the training required to formulate, design, implement, and manage a multidisciplinary cancer survivorship program.
Eligibility Requirements/Criteria (When Applicable):
1. Admission is contingent upon completion of an ACGME accredited urologic training program or an appropriate foreign program.
2. Applicant should have completed all three steps of USMLE.
3. Applicant must have three letters supporting application for fellowship. One letter must be from current program director.
4. Applicant must be eligible for a North Carolina medical license prior to starting the fellowship.
University of North Carolina
Chapel Hill, NC
View Details
Institution Name:
University of North Carolina – Chapel Hill
Fellowship Program Name:
Genitourinary Reconstruction & Gender Affirming Surgery Fellowship
Fellowship Program Location (City, State, Country)
Chapel Hill, North Carolina, USA
Fellowship Program Director Name:
Brad Figler, MD, FACS
Fellowship Program Contact Person Name:
Aleasha Crisp
Aleasha_Crisp@med.unc.edu
Fellowship Program Website Link: https://www.med.unc.edu/urology/education/fellowship-programs/genitourinary-reconstruction/
Length of Fellowship Program:
1 year
Fellowship Program Description:
The UNC Genitourinary Reconstruction and Gender Affirming surgery fellowship provides a comprehensive and unique training experience in reconstructive urology, with a focus on open and robotic repair of ureteral, bladder neck and urethral stenoses/fistulas; genital skin deficiency due to trauma, infection and cancer; and gender affirming bottom surgery. Fellows benefit from a diverse faculty, whose backgrounds include reconstructive urology, uro-oncology, and plastic surgery.
Eligibility Requirements/Criteria:
Unrestricted North Carolina Medical License, US Citizen, or permanent resident. Visa candidates may be considered in exceptional cases.
Case Log:
View Case Log
Wake Forest University Baptist
Winston-Salem, NC
View Details
Institution Name:
Wake Forest University Baptist
Fellowship Program Name:
Male Genitourinary Reconstructive Surgery Fellowship Program
Fellowship Program Location (City, State, Country):
Winston-Salem, North Carolina, USA
Fellowship Program Director Name:
Ryan Terlecki, MD, FACS
rterlecki@wakehealth.edu
Fellowship Program Contact Person Name:
Samanta Money
Smoney@wakehealth.edu
Fellowship Program Website Link:
http://www.wakehealth.edu/Urology
Length of Fellowship Program:
1 year
Fellowship Program Description:
Wake Forest School of Medicine Department of Urology is pleased to offer a fellowship in Urologic Reconstruction, Prosthetics, and Infertility. This is a one-year program under the direction of Ryan Terlecki, M.D. The fellow will also have the opportunity to work with faculty including Dr. Robert Evans, Dr. Ashok Hemal, and Dr. Alejandro Rodriguez in cases involving urinary diversion, bladder augmentation, ureteral reconstruction, etc. In addition, the fellow will be involved in international outreach.
Our department is ranked as one of the nation’s best by US News and World Report. We experience a high patient volume. Dr. Terlecki’s practice will expose the fellow to many cases involving reconstruction for urethral strictures, fistulas, Peyronie’s disease, male stress incontinence, erectile dysfunction, buried penis, ureteral strictures, and neurogenic bladder. In addition, we are on the forefront of investigating the use of tissue engineering in reconstructive surgery, and the fellow would have the opportunity to participate in research with the Wake Forest Institute of Regenerative Medicine.
In addition to working alongside Dr. Terlecki, the fellow will serve as a Clinical Instructor and, they will have the opportunity to independently manage patients in the clinic and operative settings. There will be numerous opportunities to participate in local and national meetings, as well as in the education of students, residents, and other providers. This program is designed not only to afford proficiency in the most up-to-date surgical techniques, but also to expose the trainee to the future of reconstructive medicine and equip them to serve as an educator and leader in this field.
Upon completion of the program, the fellow should be proficient in the following:
1. Fundamental principles of male urologic reconstruction and tissue healing.
2. Decision-making and surgical technique for urethral and penile reconstruction.
3. Prosthetic surgery for male incontinence and erectile dysfunction.
4. Office management of andrology and infertility.
5. Techniques for sperm harvesting and vasovasostomy.
6. Balanced scrutiny of the medical literature and the ability to plan and conduct meaningful research.
7. Understanding the science behind tissue engineering and the application to urologic reconstruction
Eligibility Requirements/Criteria (When Applicable):
1. Admission is contingent upon completion of an ACGME accredited urologic training program in the United States.
2. The applicant must be a US citizen.
3. The applicant must have three letters of support, including one from their residency program director.
4. The applicant must have passed all 3 steps of the USMLE prior to the match date and be eligible for a North Carolina license prior to starting fellowship.
Ohio
Case Western Reserve University
Cleveland, OH
View Details
Institution Name:
Case Western Reserve University/University Hospitals Cleveland Medical Center
Fellowship Program Name:
Reconstructive Urology and Gender Affirmation Surgery Fellowship
Fellowship Program Location:
Cleveland, OH USA
Fellowship Program Director Name:
Dr. Shubham Gupta
Shubham.Gupta@UHhospitals.org
Fellowship Program Contact Person Name:
Delicia Pratts Delicia.pratts@uhhospitals.org
Fellowship Program Website Link:
https://www.uhhospitals.org/medical-education/urology-medical-education
Length of Fellowship Program:
One or two years depending on the applicant’s goals. Year 1 would be clinical with outcomes based research focus. Year 2 will include the opportunity for basic sciences research, population health certification, and further sub-specialty electives.
Fellowship Program Description:
University Hospitals is excited to offer a GME approved, GURS certified fellowship with a focus on lower tract reconstruction, upper tract reconstruction, survivorship reconstruction, and gender affirmation surgery. There are 3 reconstructive urologists (Gupta, Scarberry, Mishra), and one reconstructive gynecologist (Pope) who comprise the core faculty. All of the faculty members themselves have trained at different places, thereby enriching the flavor of the fellowship. Fellows can expect to gain proficiency in simple and complex urethral stricture disease, flaps and grafts harvest, open and robotic intra-abdominal reconstruction, vaginoplasty, metoidioplasty, and phalloplasty. As the only comprehensive gender affirmation program in the region, we perform more than 100 primary genitoplasties (vaginoplasty, metoidioplasty, phalloplasty), and approximately 50 revision surgeries.
Research opportunities are plentiful, including access to several national datasets, prospective cohort studies, community based participatory research projects, and translational research with a focus on microbiome and genetic analysis. Research support exists in the form of research coordinators, statisticians, and a recon research group comprising a rotating roster of 5 medical students and residents.
Eligibility Requirements/Criteria
Unrestricted Ohio Medical License, US Citizen, or permanent resident. Visa candidates may be considered in exceptional cases.
The ideal candidate should have an interest in developing a wide breadth of surgical aptitude with a keen interest in fostering skills to become a successful surgeon scientist. We believe this program has the opportunity to cultivate talent amongst genitourinary surgeons who aim to bring research from the bench to the bedside. This will provide high level of literature to the field of reconstructive surgery and will serve as a foundation for major advancements in the discipline. Furthermore, the fellow will have an opportunity to pursue subspecialized focus in advanced men’s health training with 2 faculty members at the institute, with an additional opportunity to focus on a capstone in leadership that will prepare them to design a program in gender affirming surgery. Overall, we firmly believe that this program provides a unique opportunity to train surgeon scientists who will be groomed to be leaders at institutional, national, and international level.
Cleveland Clinic, Glickman Urological and Kidney Institute
Cleveland, OH
View Details
Genitourinary Reconstruction and Prosthetic Surgery
Program Director: Kenneth W. Angermeier, MD
Fellowship Program Length: 1 year
Fellowship Program Location: Cleveland, Ohio
Fellowship Program Director Name: Kenneth W. Angermeier, MD
Email: angermk@ccf.org
Email Alternative / Fellowship Coordinator: symonsm@ccf.org
Coordinator: Melanie Symons
Length of Fellowship Program: 1 year
This intense one-year clinical fellowship is part of the educational mission of the institute administered through the Center for Genitourinary Reconstruction. The fellow will develop a thorough understanding of the evaluation and management of a broad spectrum of disorders primarily involving the male lower urinary tract and genitalia requiring reconstructive surgery, and a keen interest in contributing to the specialty through clinical research. Clinical experience is gained through a high-volume practice of lower urinary tract reconstruction and genitourinary prosthetic surgery for urethral stricture and complex fistulas, neurogenic bladder, incontinence, erectile dysfunction, buried penis, penile and urethral cancer, and other less common conditions. Major open and robotic abdominal and pelvic cases performed include bladder neck reconstruction for refractory stricture, bladder augmentation and catheterizable stoma for neuropathic or congenital bladder anomalies, cystectomy with urinary diversion for devastating injury of the bladder or urethra, and ureteral reimplantation or reconstruction. We also have a special interest in transitional urology, providing comprehensive care for patients who have persistent problems in adolescence or adulthood related to congenital urological disorders. Finally, with the recent acquisition of new staff members, gender affirmation surgery is an increasing part of our reconstructive urology practice.
The fellowship position entails 1 day per week in clinic with center staff, one-half day of the fellow’s own clinic, and 3.5 days per week in the operating room. The fellow also is expected to participate in all weekly urology departmental conferences and to select articles for and attend monthly journal club. There is an expectation for one or two clinical research projects during the year. The fellow will also help plan and execute subspecialty-specific symposia.
Eligibility Requirements/Criteria: Fellows must be able to obtain an Ohio Medical License to become a Limited Clinical Practitioner (LCP) allowing independent practice as a component of their training.
How to apply: We participate in the AUA match for fellowships in genitourinary reconstructive surgery. Information is available on the Society of Genitourinary Reconstructive Surgeons website at societygurs.org. Applicants should send a copy of their AUA Match application, CV and two to three letters of recommendation to the contact below by the deadline indicated on the GURS website.
For any further questions or details, please email UrologyFellowship@ccf.org.
Oregon
Oregon Health & Science University
Portland, OR
View Details
Institution Name:
Oregon Health & Science University
Fellowship Program Name:
OHSU GURS & Gender-affirming Surgery Fellowship
Fellowship Program Location (City, State, Country):
Portland, Oregon USA
Fellowship Program Director Name:
Daniel Dugi, MD, FACS
Fellowship Program Contact Person Name:
Susi Driscoll
driscols@ohsu.edu
Fellowship Program Website Link:
https://www.ohsu.edu/urology/reconstructive-urology
Length of Fellowship Program:
1 year
Fellowship Program Description:
The OHSU Transgender Health Program is one of the most comprehensive and highest-volume programs for gender-affirming care in the U.S. Faculty within the Department of Urology lead the vaginoplasty and metoidioplasty programs and work in conjunction with Plastic Surgery to provide phalloplasty care.
The OHSU Department of Urology at OHSU is pleased to offer a one-year Reconstructive Urology Fellowship with emphasis on gender-affirming genital surgery and health care for board-eligible or board-certified Urologists. Candidates must have a strong interest in gender-affirming care.
The primary objective of the OHSU Urologic Reconstructive and Gender-Affirming Surgery Fellowship is to develop the unique clinical and surgical skill set required for expert management of genitourinary reconstructive problems with strong emphasis on gender-affirming genital surgery. Combined with the surgical principles of genitourinary reconstruction, the fellowship will be one of the first programs in the United States to offer dedicated surgical training in this area. The fellow will train with multiple faculty within the department of Urology (3 GURS-fellowship trained and 1 FPRMS-fellowship trained) and Plastic Surgery in reconstructive genital surgery.
Fellows participate in a monthly multi-disciplinary transgender health conference and in creation of gender-affirming clinical pathways. Fellows interact regularly with our broader program leadership and attend programmatic and surgical leadership meetings.
Fellows have a wide variety of research opportunities.
Eligibility Requirements/Criteria (When Applicable):
Candidates much supply a letter of recommendation from their training program director, as well as two other letters of recommendation. Candidates must be Board-eligible urologists at time of fellowship start and obtain a full Oregon medical license prior to start (having passed USMLE Step 1-3).
Deadline for applications: We follow the general GURS deadlines, but we offer interviews on a rolling basis, and there are limited interview opportunities. Early submission of application materials is recommended.
Strong experience with reconstructive urologic surgery in residency training is beneficial.
Pennsylvania
Fox Chase Cancer Center
Philadelphia, PA
View Details
Institution Name and Location:
Fox Chase Cancer Center
Fellowship Program Name:
Reconstructive and Prosthetic Urology Fellowship Program
Fellowship Program Location (City, State, Country):
Philadelphia, PA, USA
Fellowship Program Director Name:
Jay Simhan, MD, FACS
Vice Chair and Professor of Urology, Director of Reconstructive Urology, Fellowship Director, Fox Chase Cancer Center
jsimhan@gmail.com
Fellowship Program Contact Person Name and Email:
Ramona Guzman
Ramona.Guzman@fccc.edu
Fellowship Program Website Link:
https://www.foxchase.org/reconstructive-and-prosthetic-urology-fellowship
Length of Fellowship Program:
1 year
Fellowship Program Description:
This is a 1-year reconstructive urology fellowship offered in our Department of Urology. Unique perspectives gained through the fellowship program include comprehensive exposure to urogenital reconstruction, robotic urinary tract reconstruction, neuro-urological reconstruction, and the opportunity to develop expertise in the surgical management of erectile dysfunction/male stress incontinence.
This fellowship offers a broad range of experiences with areas of specific emphasis including urethroplasty (e.g. primary anastomosis, radiation induced strictures, substitution urethroplasty, etc.), urologic prosthesis surgery (penile implantation, revision penile implantation, artificial urinary sphincter, revision male stress incontinence surgery), male genital reconstruction/Peyronie’s disease (plication, plaque incision with grafting, STSG, scrotal reconstruction), ureteral reconstruction (robotic/open Boari, Psoas hitch, ureteral reimplant, pyeloplasty and reoperative pyeloplasty), genitourinary trauma (conservative and operative approaches to renal, bladder and genital trauma), open and minimally-invasive bladder augmentation/urinary diversions). Optional experiences in female pelvic reconstruction (pelvic organ prolapse, neuromodulation, female stress incontinence, female urethral reconstruction) are also available to the fellow. The fellow will also have the option to have an immersive experience in developing an advanced knowledge of urodynamics/video urodynamics.
The development of academic projects is strongly encouraged throughout the fellowship. In sum, the fellow will be provided with a broad range of projects that are ongoing or planned pertinent to fellowship training and a future career in academics. The fellow will be supported to present abstracts at regional, national, and international urology meetings with an ultimate goal of manuscript preparation/submission. The fellow will have attending privileges at all sites and accepts the same generous call schedule as the faculty (approximately 1 in every 19 weeks). Urology residents take first call at all sites. The fellow participates in the operating room at least 3-4 days per week. Teaching responsibilities include occasional preparation of Grand Rounds lectures, participation in the didactic aspects of the residency program, and supervising residents in the operating room.
Case Volume for Faculty
Urethral reconstruction: 115 cases/yr
Penile Prosthesis: 100 cases/yr
AUS/Sling: 75 cases/yr
Abdominal reconstruction (including robotic): 70 cases/yr
Genital reconstruction: 80 cases/yr
Female Pelvic Reconstruction: >150 cases/yr
Eligibility Requirements/Criteria
1. Applicant should be able to obtain full medical license from the state of Pennsylvania at the time of initiation of the fellowship.
2. Current CV
3. Applicant should have completed all steps of the USMLE
4. Applicant must have 3 supporting letters of recommendation (one letter must be from Chair or program director)
5. Admission is contingent upon completion of an ACGME accredited urologic training program or a similar training program from outside the United States.
Away Rotations and Trips:
The fellow is supported by the Department to attend the Annual AUA meeting, GURS Annual Meeting, the Sexual Medicine Society Meeting, the Societe Internationale d’Urologie (SIU) Annual Meeting, and the Mid Atlantic AUA Annual Meeting. Additionally, attendance in at least one international surgical workshop is supported (this is discussed/planned with the Program Director).
For any further questions or details, please email: Jay Simhan, MD, FACS (jsimhan@gmail.com)
Tennessee
Vanderbilt University Medical Center
Nashville, TN
View Details
Institution Name:
Vanderbilt University Medical Center
Fellowship Program Name:
Genitourinary Reconstruction and Trauma Fellowship
Fellowship Program Director:
Niels V Johnsen MD MPH FACS
niels.v.johnsen@vumc.org
Fellowship Program Contact:
Megan Walker
Meagan.fathera@vumc.org
Fellowship Website:
https://www.vumc.org/urology/education-genitourinary-reconstruction-and-trauma-fellowship
Length of Fellowship: 1 year
Fellowship Program Description:
The Vanderbilt Genitourinary Reconstruction and Trauma Fellowship is a mentored, graduated training experience providing comprehensive training in the diagnosis and management of male and female reconstructive urologic conditions. With 4 core fellowship faculty (Niels Johnsen, Melissa Kaufman, Elisabeth Sebesta, and Roger Dmochowski), fellows will experience the true breadth and depth of all aspects of genitourinary reconstruction and injury management. Furthermore, as the only quaternary referral center in the region, as well as the only Level I trauma center, Vanderbilt provides extensive opportunities for fellows to manage complex and unique patient conditions.
The clinical training encompasses all aspects of reconstruction for both men and women, as well as gender affirming surgery, through widespread surgical training in open, robotic, and transvaginal approaches. On the male reconstructive front, we offer extensive opportunities in anterior and posterior urethral reconstruction and rectourethral fistulae repair utilizing gracilis or other muscle flaps. Genital reconstruction is performed for lymphedema, hidradenitis, buried penis, genital malignancies, and following necrotizing soft tissue infections, where fellows will gain expertise in the utilization of various skin grafting and fasciocutaneous flap techniques. Fellows will also be exposed to a large clinical practice of post-prostatectomy incontinence and erectile dysfunction, as well as Peyronie’s disease.
The female pelvic health and voiding dysfunction component of the fellowship continues the great legacy of the Vanderbilt Female Pelvic Medicine fellowship initially founded by Roger Dmochowski in 2003 by providing unparalleled training in the management of female genitourinary reconstruction. Fellows gain extensive experience managing urinary incontinence and overactive bladder, voiding dysfunction, neurogenic bladder, genitourinary fistula and diverticula repair, pelvic organ prolapse, pelvic floor dysfunction, and neuromodulation. Procedures are performed both through transvaginal and transabdominal approaches, both robotic and open, preparing fellows to manage these conditions utilizing a variety of techniques.
Fellows will also gain extensive experience in the surgical management of bladder and upper tract reconstruction through robotic bladder neck reconstruction, bladder augmentation, open and robotic ureteral reconstruction, ileal ureter creation, as well as both continent and incontinent urinary diversions. Lastly, fellows have the opportunity to participate in our growing gender-affirming care program in conjunction with plastic surgery in vaginoplasty, metoidioplasty, and phalloplasty procedures.
Acute management and long-term survivorship care of genitourinary injury patients is a major component of the fellowship. With a graduated autonomy experience, fellows will direct the conservative and surgical management of GU trauma patients, coordinating closely with the general surgery and orthopaedics trauma teams.
The primary goal of the fellowship is to train future leaders in the world of reconstructive urology. Fellows are expected to complete scholarly work and contribute to the academic mission of the department by participating in Departmental conferences and didactics. Fellows are mentored through the development of research protocols, study design, statistical analysis and research dissemination and are expected to present their work at societal and national meetings.
Eligibility Requirements:
1. Must be eligible for medical licensure in the state of Tennessee prior to starting fellowship.
2. Admission is contingent upon completion of an ACGME accredited urologic training program.
3. Applicants should have completed all 3 steps of USMLE.
4. Applicants must send a cover letter, current headshot, current CV, and three reference letters supporting their application. One of these must be from the residency program director and/or department chairperson.
Texas
Baylor Scott and White All Saints Medical Center
Fort Worth, TX
View Details
Institution Name:
Baylor Scott and White All Saints Medical Ctr
Fellowship Program Name:
BSW Genitourinary Reconstruction Fellowship
Fellowship Program Location (City, State, Country):
Fort Worth, Texas, USA
Fellowship Program Director Name:
Charles L. Secrest, MD, Director, BSW Center for Reconstructive Urology, graduated fellowship EVMS 1992, in practice 30 years.
Fellowship Program Contact Person Name:
Charles L. Secrest, MD
secrestGUrecon@gmail.com
Fellowship Program Website Link:
www.bswhealth.com/reconstructiveurology
Length of Fellowship Program:
1 year
Fellowship Program Description:
This is a very busy clinical fellowship in both male and female genitourinary reconstruction. The mainstay of our male cases include excision of Peyronies plaque w autologous dermal grafting, tunica plication, all types of male urethroplasty and bladder neck reconstruction, hypospadias repair, prosthesis surgery both penile and AUS including complex redo cases, plus complex fistula repairs both male and female. We perform more male than female surgeries but the fellow will finish this program well trained in female pelvic medicine and reconstructive surgery including all types of slings, mesh removal and reconstruction, repair of cystocele, rectocele, enterocele and vaginal prolapse. Other female cases include urethroplasty, diverticulectomy, urethral construction with local flaps, and transvaginal urethral closure with diversion. We now perform mostly robotic surgery for all abdominal procedures. We operate on Tuesday, Thursday, and Friday. This program is an apprenticeship in reconstructive urology with a lot of hands on teaching and a very strong clinical experience. I look forward to meeting you and discussing our program in more detail. Please call or send an email to make arrangements for a visit to Fort Worth!
Eligibility Requirements/Criteria (When Applicable):
Board eligible ABU, Fellow must be able to obtain an unrestricted Texas Medical License after completing a urology residency, 3 letters of recommendation, CV, letter of interest.
University of Texas Southwestern
Dallas, TX
View Details
Institution Name:
University of Texas Southwestern
Fellowship Program Name:
Urologic Trauma, Reconstruction, and Prosthetics
Fellowship Program Location (City, State, Country):
Dallas, Texas, USA
Fellowship Program Director:
Steven J. Hudak, MD, FACS
Professor of Urology
Distinguished Chair in Reconstructive Urology,
In Honor of Allen F. Morey, MD
Director, Urology Residency Program
Steven.Hudak@utsouthwestern.edu
Fellowship Program Contact Person Name:
Shareef Hamad
Shareef.Hamad@UTSouthwestern.edu
Fellowship Program Website Link:
https://www.utsouthwestern.edu/education/medical-school/departments/urology/education-training/fellowships/urologic-trauma.html
Length of Fellowship Program:
1 Year
Fellowship Program Description:
The Urologic Trauma, Reconstruction, and Prosthetics fellowship at UT Southwestern is a robust one-year clinical program with the objective of creating the next generation of leaders in the field of genitourinary reconstructive surgery.
Clinical training encompasses all aspects of upper and male lower genitourinary tract reconstruction, including urethral reconstruction, male incontinence and erectile dysfunction, ureteral reconstruction, robotics, urinary diversion, and repair of complex male genitourinary deformities, including Peyronie’s disease, urinary fistulae, and buried penis. Many cases involve a multidisciplinary care team with urologic oncologists and colorectal, plastic, and burn surgeons. Prosthetic cases focus on erectile dysfunction and incontinence and are performed in unusually high volumes.
UT Southwestern is the only urology residency training program in the DFW area and the largest urology training program in Texas. The fellow will gain extensive operating experience working with two reconstructive GU surgeons at four affiliated teaching hospitals – Clements University Hospital, Dallas County’s Parkland Memorial Hospital, Fort Worth’s John Peter Smith Hospital, and Children’s Medical Center, Dallas. Fellows will also gain valuable teaching skills as they often operate in the role of junior faculty surgeon when operating with urology residents.
There is no required call or general urology “fellow clinic” obligations. Abundant clinical research opportunities are available, given our extensive institutional databases capturing nearly 20 years of GU reconstruction data. Most fellows graduate with numerous publications and present at multiple national meetings (with fully funded travel). Time commitment during the fellowship is approximately 90% clinical and 10% research.
Eligibility Requirements/Criteria (When Applicable):
Applicants must have completed an ACGME-accredited Urology residency, as well as be eligible to receive a Texas Medical License.
Utah
University of Utah
Salt Lake City, UT
View Details
Institution Name:
University of Utah
Fellowship Program Name:
Genitourinary Injury and Reconstructive Urology
Fellowship Program Location (City, State, Country):
Salt Lake City, Utah, USA
Fellowship Program Director Name:
Jeremy Myers, MD
Fellowship Program Contact Person Name:
Elizabeth Royall
Elizabeth.Royall@hsc.utah.edu
Fellowship Program Website Link:
https://medicine.utah.edu/surgery/urology/education/fellowships/reconstructive/
Length of Fellowship Program:
2 Years
Fellowship Program Description:
The fellowship is 2-years. The first year is spent with a research focus, however, the fellow will be clinically active for 2 days of the week. The second year is clinically focused, and the fellow will spend 3 or 4 days in clinical work during week. There will be an opportunity to achieve a Master of Science Clinical Investigation (MSCI) or similar degree (MBA, Masters of Education) during the 1st and 2nd years depending upon the fellow’s goals.
The fellowship emphasizes operative experience, teaching, and research. Operative experience encompasses the full-breadth of reconstructive urology and there will be ample opportunity to become well-versed in urethroplasty, posterior urethroplasty, urinary diversion, augmentation cystoplasty, incontinence treatments, buried penis, and gender affirmation surgery (both transmasculine and transfeminine surgery). An important part of the fellowship is an emphasis on learning how to teach in the OR. As fellowship responsibilities progress so does teaching experience in the operating room with residents. University of Utah has a robust health services, basic science, and clinical outcomes research programs. There are opportunities for grant writing workshops, statistical analysis, and research mentorship in a number of different areas in reconstructive urologic research. Currently we have active projects utilizing the Trauma and Urologic Network of Surgeons, the Neurogenic Bladder Research Group, the National Trauma Databank, the Trauma Quality Improvement Project, and the Utah Population Database. Fellows identify the most interesting projects that match their interest and have active mentorship in developing these ideas.
Eligibility Requirements/Criteria (When Applicable):
Graduate of US urology residency program or eligible for US medical licensure
Washington
University of Washington
Seattle, WA
View Details
Institution Name:
University of Washington
Fellowship Program Name:
Genitourinary Trauma and Reconstruction Fellowship
Fellowship Program Location (City, State, Country):
Seattle, Washington, USA
Fellowship Program Director Name:
Hunter Wessells, MD, FACS
wessells@uw.edu
Fellowship Program Contact Person Name:
Amy Say
urofellow@uw.edu
Fellowship Program Website Link:
https://urology.uw.edu/education/fellowship/trauma
Length of Fellowship Program:
1 year
Fellowship Program Description:
The University of Washington trains academic leaders in reconstructive urology. The fellowship, in its 19th year, continuously evolves in response to needs of patients and learners, and advances in surgery and technology. Building on a foundational understanding of injury mechanisms, ranging from acute trauma to the delayed effects of ionizing radiation and surgery, the program retains a significant focus on anterior and posterior urethra reconstruction. Additional emphasis areas include management of acute genitourinary injuries, genital reconstruction, and robotic upper and lower urinary tract surgery. The Fellow works closely with UW Medicine faculty members Hunter Wessells, Judith Hagedorn and Alexander Skokan, and Army urologist Jonathan Wingate. A structured educational program includes weekly conferences and daily interaction with urology residents, advance practice providers, and medical students. Surgical collaborations on complex reconstructive cases involve faculty in Trauma, Orthopedic, Colorectal and Plastic Surgery as well as a multidisciplinary gender affirming genital surgery program. Experience with implants for ED and male urinary incontinence, rectourethral fistulae, Peyronie’s disease and urinary diversion completes the training. A portion of the Fellowship is devoted to scholarship. Fellows are encouraged to take advantage of the resources of the Urology Research Outcomes Collaborative and Harborview Injury Prevention and Research Center.
Graduates have advanced in academic departments, cancer centers, and community practice. Significant contributions to the field of GU trauma and reconstruction include their participation in AUA Guidelines, the TURNS Network, AUA Core Curriculum, as well as through NIH funded grants and leadership of centers of excellence in gender affirming surgery and fellowship programs.
Eligibility Requirements/Criteria (When Applicable):
1. Admission is contingent upon completion of an ACGME-accredited urologic training program or an appropriate foreign program.
2. The applicant must have a letter of support from their urology training program director recommending them for the fellowship and attesting to the candidate’s successful completion of the urology training program. Two additional letters of recommendations are required.
3. The applicant should have completed all 3 steps of USMLE and be eligible for a WA State license prior to starting fellowship.
Programs in Probation
Virginia
Eastern Virginia Medical School
Virginia Beach, VA
View Details
Fellowship Program Name: Adult & Pediatric Genitourinary Reconstructive Surgery
Fellowship Program Location: Virginia Beach, VA, USA
Program Director: Kurt A. McCammon, MD, FACS
urology_dept@evms.edu
Fellowship Coordinator:
Ms. Lynn Vass
Email: vasslm@evms.edu
Phone: (757) 452-3459
Fax: (757) 961-4099
Mailing Address: Eastern Virginia Medical School
225 Clearfield Avenue
Virginia Beach, Virginia 23462
Length of Fellowship Program: 1 Year
Prerequisite/Eligibility Requirements:
- This fellowship is open to both U.S. and non-U.S. citizens as well as to foreign
medical graduates with valid ECFMG certification. Eastern Virginia Medical
School supports J-1 visas for our Fellows. - Applicant must have completed urology residency training
- Applicant should have completed Step1, Step 2 CK, and Step 2 CS of USMLE
- Interested applicants should submit their application, CV, personal statement, photo, and 3 letters of recommendation – one letter from residency program director
Program Description:
The Fellowship involves surgery for disorders of the male and female genitourinary tract, and in many cases the external genitalia, stemming from congenital anomalies, trauma, inflammatory disorders, and in the case of the female, incontinence and pelvic descensus. Individuals completing fellowship training should demonstrate knowledge, skill, and understanding of the basic medical sciences relevant to the genitourinary tract, and in specific the external genitalia. These skills include female pelvic reconstructive surgery which includes disorders of incontinence and pelvic descensus. Many of the disorders involving the male genitalia are closely coupled to disorders of erectile function. Thus fellowship training is designed to educate physicians in the clinical aspects of diagnosis, medical and surgical therapy, and the prevention of and reconstruction for these disease processes.